Outpatient Department Instruments
Summary:
This Outpatient Department Instruments note describes various instruments used in eye exams and vision tests, including Snellen’s chart for checking distant vision, pinhole testing for detecting a refractive error, and retinoscopes for detecting media opacity. The text also discusses ophthalmoscopes for examining the fundus and diagnosing eye conditions, and Goldman applanation tonometers for measuring intraocular pressure to diagnose and monitor glaucoma. Other instruments mentioned include the slit lamp biomicroscope and the Goldman triple mirror contact lens, which are used for a variety of diagnostic and therapeutic purposes.
Excerpt:
Outpatient Department Instruments
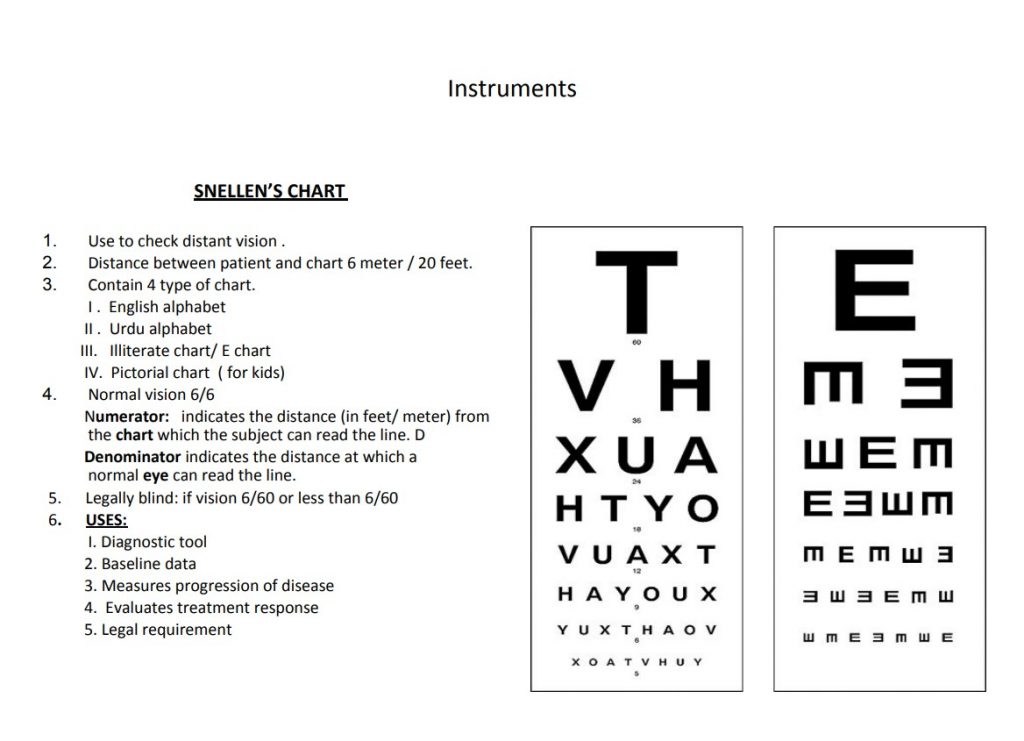
SNELLEN’S CHART
1. Use to check distant vision.
2. Distance between patient and chart 6 meters / 20 feet.
3. Contain 4 types of chart.
I . English alphabet
II . Urdu alphabet
III. Illiterate chart/ E chart
IV. Pictorial chart ( for kids)
4. Normal vision 6/6
– Numerator: indicates the distance (in feet/ meter) from the chart from which the subject can read the line. D
– Denominator indicates the distance at which a normal eye can read the line.
5. Legally blind: if vision is 6/60 or less than 6/60
6. USES:
I. Diagnostic tool
2. Baseline data
3. Measures progression of the disease
4. Evaluates treatment response
5. Legal requirement
Equipment required for the vision test
1. Multi-letter Snellen
2. Plain occluder,
3. Pinhole occluder
4. Patient’s glasses
Procedure:
1. Well-illuminated room and Snellen’s chart.
2. Patient and chart distance 6 meters.
3. Test the eyes one at a time, at first without any spectacles (if worn).
4. Occlude one eye with an occluder.
5. Ask the patient to read from the top of the chart.
6. If the patient cannot read the largest (top) letter at 6 meters, reduce the distance to 1 meter till the patient can see.
7. able to read at 1 meter (1/60): CF
8. If the patient cannot count fingers: Hand movements (HM): VA = HM
9. perception of light’ (VA = PL).
10. If they cannot, record ‘no perception of light’ (VA = NPL).
11. After testing without any correction, test the patient while wearing any current distance spectacles and record the VA in each eye separately, with correction.
12. If vision is not improving with/without spectacles, then do a PIN HOLE TEST

Reviews